Overview: What’s A Molar Pregnancy & How Common Is It?
A molar pregnancy is an uncommon pregnancy complication. It only happens in around 60-120 of 100,000 pregnancies in North America and Europe. However, it might occur more frequently in other countries. Some women have a higher risk, including older women and in some cases, those with one or more previous molar pregnancy histories. (1)(2)(3)
This pregnancy complication is also called a hydatidiform mole. (1)(3)
It’s one of the lesser-known pregnancy complications, and often you might not even have heard about it until it happens to you or someone you know. Experiencing a molar pregnancy can be disheartening and stressful. It can take a toll on your body, mind, and emotional state.
We’ve written this article to help shed a better light on this rare condition, and hopefully by the end of this article, you’ve gained a better understanding of it.
There are two types of molar pregnancy: complete and partial. Both are caused by a genetic error during fertilization. An abnormal placenta grows in both types: (1)(2)(3)
There’s no fetus in a complete molar pregnancy. (1)(2)(3)
There might be some fetal development in a partial molar pregnancy. (1)(2)(3)
Abnormal tissues from the placenta might look like grape-like clusters (cysts) on an ultrasound scan. These molar tissues often don’t sustain normal fetal ’ growth (if a fetus is present). The fetus may also present with genetic abnormalities even if a properly formed placenta is present. This situation can lead to a miscarriage in early pregnancy. (1)
In this article, we’ll cover the main causes of molar pregnancy, the two different types, possible signs and symptoms, and much more. Keep reading to find out.
What Is Gestational Trophoblastic Disease (GTD)?
This is a group of diseases characterized by the development of rare tumors during pregnancy. Often, the tumors begin in the cells that are supposed to become the placenta, the source of nutrition for the growing embryo. The tumors can either be cancerous (malignant) or noncancerous (benign). (1)(3)
Molar pregnancy is a form of GTD. Most of the time, it’s considered benign. However, it can also become invasive and malignant. That’s why monitoring is essential for about a year after a molar pregnancy. (1)(3)
GTDs are unique because they don’t form directly from the mother’s tissues. Instead, they’re from the gestational or placental tissue. (3)
Other forms of GTDs: (3)
- Placental site trophoblastic tumors
- Gestational choriocarcinoma (a life-threatening cancerous growth that can be extremely invasive and malignant)
What Are The Main Causes Of Molar Pregnancy?
- Abnormal fertilization of the egg or oocyte (1)(2)
There are two sets of genes or chromosomes in a normal conception: one is from the father and the mother. The combination creates a viable fetus. (see image below)
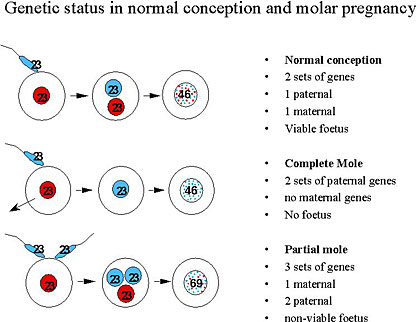
However, genetic anomalies at fertilization can lead to a molar pregnancy. (1)(2)(3)
Instead of two sets of chromosomes from the mom and dad, the fertilized egg might carry two sets of genetic materials from the dad or even three sets of genes (one from the mother and two from the dad). These can be differentiated by the two types of molar pregnancies discussed in the next section. (1)(2)(3)
It’s important to note that a molar pregnancy cannot be prevented.
What Are The Types Of Molar Pregnancies?
Molar pregnancies can either be “complete mole” or “partial mole.” (1)(2)(3)
Things To Know About A Complete Molar Pregnancy
Conditions in a complete mole: (1)(2)(3)
- Abnormal placenta (a mass of rapidly growing, abnormal cells that develop into fluid-containing tumors ) with a “snowstorm” appearance on the ultrasound scan
- No embryo development
- Typically produces higher hCG levels (usually 100,000+) than the normal range for the specific gestational age
- The original nucleus with the mother’s genetic material becomes lost (either while the egg is still developing in the ovary or at conception)
- The fertilized egg’s genetic material is only from the father; happens when an enucleated egg (without a nucleus) is fertilized by two sperm or the sperm that duplicates at fertilization
- The uterus or womb is usually larger than the usual size based on the expected gestational date
- There’s around 10-15% chance that you might need further treatment after a complete molar pregnancy diagnosis and treatment (e.g., evacuation or D&C; discussed below)
- The risk of invasive disease or cancer complication is around 15% to 20% in a complete molar pregnancy.
Things To Know About A Partial Molar Pregnancy
Conditions in a partial mole: (1)(2)(3)
- Abnormal placenta with a “Swiss cheese” appearance on the ultrasound scan
- Some embryonic development (but the embryo doesn’t develop much and is highly unlikely to survive); in some rare cases, a heartbeat might be detected, but this is very unlikely
- Typically has similar or less hCG levels than the normal range for the specific gestational age
- Genetic material present from both parents but with an imbalance; it happens when there are two sets of chromosomes or genetic material from the father because the egg was either fertilized by two sperm or a normal sperm duplicates while fertilizing an egg
- The uterus or womb is usually larger than the usual size based on the expected gestational date
- Most partial molar pregnancies don’t require any additional intervention after the initial treatment (e.g., evacuation or D&C; discussed below), because over 99% of the residual cells are likely to die away over the following weeks
- As many as 15-60% of partial mole cases may be diagnosed as a missed or incomplete miscarriage
- The risk of invasive disease or cancer complication is around 1% to 5% in a partial molar pregnancy.
Signs & Symptoms Of A Molar Pregnancy
Possible signs and symptoms that you might have a molar pregnancy: (1)(2)(3)
- Vaginal bleeding in early pregnancy (first trimester) that looks like prune juice
- Abnormal womb growth in pregnancy, whether smaller or bigger than usual
- Severe nausea and vomiting (possibly due to the higher levels of hCG hormones in the blood)
- Hyperthyroidism-like symptoms (e.g., loose stools or diarrhea, rapid heart rate, heat intolerance, restlessness, nervousness, tremors or trembling hands, unexplained weight loss, or warm and moist skin); this usually appears around 14 to 16 weeks of pregnancy
- Preeclampsia-like symptoms within the first trimester and/or early second trimester (e.g., high blood pressure with swelling in your ankles, legs, and feet); this is more likely a sign of molar pregnancy because preeclampsia rarely happens this early in normal pregnancy (it typically happens at 34+ weeks or the third trimester)
As many as 84% of molar pregnancy cases cause bleeding during the first trimester. This happens because the molar tissues begin to separate from the decidua (part of the endometrium or uterine wall). (3)
In rare cases, a molar pregnancy can also cause severe respiratory distress or breathing difficulty. (3)
Is It Possible To Have No Symptoms With A Molar Pregnancy?
Yes. Sometimes, a molar pregnancy doesn’t exhibit any symptoms. It might easily pass off asan early pregnancy miscarriage or be mistaken for a chemical pregnancy. (3)
In many of these cases, the molar pregnancy is only diagnosed after a pathology test (examination of tissues from the body) is done to identify the fetal tissue from the miscarriage sample. (3)
Can You Tell You Have A Molar Pregnancy With Your Symptoms?
Most of the time, no. However, if your vaginal bleeding has grape-like clusters and has a similar color as prune juice, then this might be a tell-tale sign of a molar pregnancy. (3)
In most cases, however, the only way to tell for certain is to see your doctor and undergo the diagnostic tests. (see below)
Finding Help & Seeing Your Doctor
When To See A Doctor For A Possible Molar Pregnancy
It’s ideal to see your doctor immediately if you experience any symptoms of a molar pregnancy or any possible pregnancy complication, for that matter.
A molar pregnancy might be rare, but it can lead to bleeding, malignant tumors, or other complications. It’s best to have the condition and its possible complications treated or managed as soon as possible to reduce serious risks. (1)(2)(3)
Preparation For Your Doctor’s Appointment
There aren’t any special preparations you need to do to visit your doctor. There’s no need to fast or visit your doctor with an empty stomach.
However, you must follow the instructions on having a full or empty bladder during the ultrasound procedure. If needed, instructions will also be given to prepare for the other tests or diagnostic procedures.
It’s also ideal to come prepared with a list of things your doctor might want to know or questions you wish to ask during your appointment.
What Your Doctor Needs To Know
Symptoms Experienced
- Make a list of the symptoms you’ve experienced
Key Personal Information & Medical History
Make a list of: (3)
- Previous miscarriages or births, if any
- Recent and past medical procedures
- Personal medical history
- Family history of molar pregnancy
Medications Taken (Includes Supplements & Vitamins)
Make a list of all your: (3)
- Medications
- Vitamins
- Supplements
LMP (Last Menstrual Period) Date
This helps: (3)
- Determine the pregnancy’s gestational weeks
- Check and compare for possible deviations in your pregnancy’s progress versus a normal pregnancy
Questions To Ask Your Doctor
- Do you think my symptoms indicate that I have a molar pregnancy?
- What type of molar pregnancy do you suspect I have?
- What tests should I undergo, and when should I get them done?
- Are there restrictions that I need to be aware of?
- What treatment options do you recommend for my condition?
- How serious is my situation?
- Are my risks of getting cancer high?
- Do you have recommendations for reading materials or other information I should know about molar pregnancy?
- Do you have any resources to support my emotional and mental health given this diagnosis?
Expectations: What Your Doctor Might Do Or Recommend
Your healthcare provider will likely perform and recommend the following: (1)(3)
- Take your medical history (and the other information listed above)
- Perform a pelvic examination (to check for discrepancies in the womb size versus the gestational or pregnancy weeks)
- Use a stethoscope to look for a heartbeat
- Request a pregnancy test (if you haven’t done this previously), transvaginal or abdominal ultrasound scan, and other necessary diagnostic tests (see below)
Where Else Can You Find Help For A Molar Pregnancy?
Aside from your OB/GYN, you might also need the following: (1)(3)
- Gynecological oncologist (if a cancerous growth is suspected)
- Emotional and mental health support, counselor, or therapist
- Hospital or diagnostic laboratory (for continued hCG monitoring)
Detection & Diagnosis Of Molar Pregnancy
How Early Can You Detect Molar Pregnancy?
The situation varies among women and in different pregnancies. It’s likely for affected women to learn they have a molar pregnancy during their first visit to the OB/GYN or after a miscarriage. (1)(2)(3)
A complete molar pregnancy can be easier to detect during early pregnancy because of the absence of an embryo (the most important clinical sign of a pregnancy). (1)(2)(3)
Tests & Diagnosis
Tests that your doctor might request to determine if you have a molar pregnancy and/or possible complications: (1)(3)
- Pregnancy blood test for hCG (human chorionic gonadotropin, the pregnancy hormone)
- Vaginal or abdominal (pelvis) ultrasound
- Chest x-ray
- CBC (complete blood count)
- CT scan (computed tomography) – provides cross-sectional images of affected areas
- PET scan (positron emission tomography) – checks for biochemical function
- MRI (magnetic resonance imaging) of your abdomen
- Blood clotting tests
- Kidney function test
- Liver function test
- Thyroid panel (to check for possible hyperthyroidism)
Ultrasound For Molar Pregnancy Detection
The abnormal cells from the molar pregnancy can have a snowstorm or grape-like appearance on the ultrasound image. Your doctor can recognize these abnormalities because they look different from normal placental tissue. (1)(3)
Depending on the type of molar pregnancy, your ultrasound may or may not show some form of fetal development. (1)(3)
The following are usually absent in an ultrasound scan for a complete mole but may be present in a partial mole: (3)
- Amniotic fluid
- Fetus (with or without a heartbeat)
What Are The Treatment & Management Options For Molar Pregnancy?
Dilation And Curettage (D&C)
This medical procedure removes the abnormal tissues, undeveloped fetus, and other pregnancy-related masses from your womb. (1)
Suction aspiration (a suction cup removes the contents of your uterus) can also be used for the D&C procedure. (1)
Uterus Removal Or Hysterectomy
This procedure involves removing the entire uterus. It’s done if the abnormal tissues from the molar pregnancy are causing a serious complication in your uterus. It’s also an option for older women who no longer want to get pregnant. (1)
However, there’s still a risk for metastatic disease or cancerous tumors even if the patient’s uterus is removed. (3)
Management Of Other Symptoms
In rare cases, you might also experience seizures or other serious and life-threatening complications or symptoms with a molar pregnancy. Your condition must be stabilized before a direct molar pregnancy treatment (such as a D&C) can be performed. (3)
Examples include: (3)
- Seizures (late-stage symptom of pre-eclampsia) with the administration of magnesium sulfate and benzodiazepines
- Breathing difficulties from pulmonary edema or respiratory distress
- High blood pressure with appropriate medications to reduce and stabilize the blood pressure
- Severe anemia or blood loss with a blood transfusion
- Hyperthyroidism using beta-blockers
- Rh(D) negative patient (mother) needs anti-D immunoglobulin administration
The D&C or hysterectomy procedures are only done once the patient’s condition is stabilized. (3)
Follow-Up Care & Continued Pregnancy Hormone hCG Monitoring
Even after the pregnancy is terminated, your doctor might recommend continued hCG monitoring. It helps your healthcare provider determine if the abnormal tissues didn’t grow back. (1)
If the hCG levels remain elevated even after the molar pregnancy has been terminated, this could be a sign of a possible cancerous or invasive condition. (3)
Weekly hCG monitoring might be recommended until the levels become undetectable. (3)
Getting pregnant during this monitoring period can affect your test results (because pregnancy raises your hCG levels). So, your doctor is also likely to recommend using a reliable contraceptive to avoid another pregnancy. (1)
Women who get pregnant right after a molar pregnancy may also have a high risk of experiencing another one. (1)
What Are The Possible Risk Factors For A Molar Pregnancy?
Maternal Age
- Older women (geriatric pregnancy); this increases molar pregnancy risks by five to ten times (1)(3)
- Younger women (early teenage years or younger than 20) (3)
Previous Molar Pregnancy
You have a 1-2% chance of experiencing a molar pregnancy if you’ve had a previous molar one. (1)(3)
Thankfully, that’s a small percentage. Most women who had a molar pregnancy can have a healthy baby in the future. (1)(3)
Your risks of molar pregnancy are higher (around 15-20%) when you’ve had two or more previous molar pregnancies. (11)
Other Risk Factors
The following can also increase your risk of molar pregnancy: (3)
- Smoking
- Diet (e.g., lower intake of the vitamin A precursor carotene and animal fats)
- Infertility (e.g., different fertility problems)
- Previous miscarriages or spontaneous abortions
- Asian race
Some studies have shown that Asians have a higher risk factor for a molar pregnancy. (4)(5)
For example, a 2016 Gynecologic Oncology study conducted in the US showed that Asian women may have a higher risk of developing complete mole than Caucasian women. However, they have a lower risk of developing partial moles. (4)
The study had similar results to earlier research (2003) published in the British Journal of Obstetrics and Gynaecology journal conducted in Northern England and North Wales. This older study showed that Asians may be 1.95 times more likely to develop gestational trophoblastic disease than non-Asians. (5)
A 2016 study also showed the following risk assessment results: (4)
- African Americans have a significantly lower risk of developing partial mole than Caucasians, but they only have a marginally less likely risk of developing a complete mole
- Hispanics have a lower risk of developing complete or partial mole than Caucasians
Outlook: What Happens If You Have A Molar Pregnancy
Prognosis: Is A Molar Pregnancy Life-Threatening?
Most molar pregnancies are benign (noncancerous). They aren’t life-threatening unless there’s a serious bleeding complication. (1)
The mole usually responds well to D&C, medications, chemotherapy, and other treatment options. (1)
Even if they’re rare, however, molar pregnancies that turn into choriocarcinoma can be life-threatening. It’s a fast-growing type of cancer but is often treated with chemotherapy. (1)
How Long Can A Molar Pregnancy Last?
A molar pregnancy doesn’t last past the first trimester. However, molar tissues and cells can persist for months – so, continued monitoring is essential. (3)
Molar Pregnancy & A Healthy Pregnancy
Can A Molar Pregnancy Become A Healthy Baby?
A molar pregnancy isn’t expected to grow and become a healthy baby, especially because the fertilized egg usually contains genetic defects.
However, the fetus might be genetically normal (with only one set of each genetic material from their parents) in some really rare cases of molar pregnancy. (1)
When this happens, the partial molar pregnancy can continue. However, this remains a very high-risk pregnancy and must be discussed with your OB/GYN. Risks you can experience during this pregnancy: (1)
- Bleeding
- Blood pressure problems
- Premature delivery and complications
Twin Pregnancy: Can You Have A Healthy Baby With A Molar Pregnancy?
Molar pregnancies are even more rare with twins, occurring once in every 20,000 to 100,000 pregnancies. (6)
Most cases of twin molar pregnancies end in a miscarriage or various complications, including fetal malformations, hyperthyroidism, and preeclampsia. (6)
However, there have been cases of healthy babies born with a molar twin. (6)
For example, a 2023 Case Reports in Women’s Health review detailed the case of a 40-year-old Caucasian woman who delivered a healthy baby that coexisted with a partial mole. The woman hadn’t experienced pregnancy complications. The baby also didn’t have complications. (6)
Still, other studies showed that most cases of a twin pregnancy with a partial or complete mole end up in complications. (7)
A 2022 BMC Pregnancy and Childbirth study reviewed cases of twin pregnancies with one molar and one viable fetus. Half of the cases reported vaginal bleeding. Three of the 12 pregnancies resulted in the birth of a baby, but one died of congenital malformations after five months. (7)
Can You Still Have A Healthy Baby After A Molar Pregnancy?
Yes. Most women who’ve had a molar pregnancy go on to have a healthy pregnancy and baby afterward. (1)(2)
Will A Molar Pregnancy Cause Infertility?
Fertility isn’t likely to be affected by a molar pregnancy unless you opt for or had to undergo a hysterectomy (uterus removal). (1)(2)
Will A Molar Pregnancy Affect Future Pregnancies?
It depends. In most cases, a molar pregnancy doesn’t affect future pregnancies, especially if the next one is after the 1-year hCG monitoring period (to check for persistent problems). (1)(3)
What Are The Risks Of Another Molar Pregnancy In The Future?
Women who have had a molar pregnancy have a 1-2% chance of experiencing it again. (1)(3)
Possible Molar Pregnancy Complications
Persistent Gestational Trophoblastic Neoplasia (GTN)
Some characteristics of this condition: (9)
- Persistently elevated hCG levels
- Usually, a lack of symptoms
- Can metastasize (spread) to the lung, liver, and other organs
Persistent Trophoblastic Disease (PTD) Or Invasive Mole
Some characteristics of this condition: (10)
- Persistently elevated hCG levels due to abnormal tissues remaining in the womb
- Anemia
- Abdominal swelling
- Vaginal bleeding
Choriocarcinoma (A Type Of Cancer)
Placenta tissue or cells left behind after a molar pregnancy have the potential to become malignant or cancerous. The condition begins in the womb but can spread to other organs. (10)
The risk of invasive disease in a complete molar pregnancy is around 15% to 20%, and in a partial molar pregnancy is 1% to 5%. (3)
This rare condition can occur in one out of around 50,000 pregnancies. (10)
Other Molar Pregnancy Complications
Some of the possible cause complications you might experience with a molar pregnancy: (1)(3)(8)
- Hemorrhage (excessive bleeding), which might require a blood transfusion
- Preeclampsia
- Thyroid problems
- Recurrent molar pregnancy
- Side effects of anesthesia if surgery is performed (e.g., nausea and vomiting, chills, bladder problems, confusion, delirium, itching, hematoma or bleeding under the skin, and/or nerve damage)
- Anemia (deficiency of healthy red blood cells, particularly when there is bleeding or hemorrhage)
- Progress to invasive molar disease or a type of cancer called choriocarcinoma (discussed above)
How To Prevent A Molar Pregnancy
There isn’t any way to prevent a molar pregnancy except trying to reduce the risk factors (e.g., quit smoking). (1)(3)
Coping With A Molar Pregnancy & Finding Support
Emotional Outlook After A Molar Pregnancy
Even though there isn’t an embryo or fetus in many cases of molar pregnancy, it’s still considered a pregnancy. It’s okay to grieve a molar pregnancy.
However, it’s also normal to feel confused over how to feel, especially if you only learned about the pregnancy after a miscarriage.
Seeking Support For A Molar Pregnancy
- Family, friends, and loved ones
- Your OB/GYN
- Mental health counselor
- Emotional support groups (such as compassionatefriends.org and nationalshare.org)
- Miscarriage support groups (such as emptyarmsbereavement.org/miscarriage-support-group and postpartum.net/get-help/loss-grief-in-pregnancy-postpartum/)
FAQs
Is A Molar Pregnancy Considered A Type Of Miscarriage?
No. A molar pregnancy isn’t a miscarriage – it’s a type of pregnancy. However, it usually leads to pregnancy loss.
Is A Molar Pregnancy A Serious Medical Emergency?
No. Most cases of molar pregnancies aren’t life-threatening unless you have bleeding complications. (1)
What Can We Resume Sex After A Molar Pregnancy?
You can resume sex anytime you’re comfortable. However, your doctor might recommend birth control to ensure you don’t get pregnant within the extended hCG monitoring period.
Other Pregnancy Topics & Concerns
- Pregnancy guide
- Acupressure for labor and delivery
- Anemia during pregnancy
- Birth affirmations
- Birth doula
- Blood pregnancy test
- Breathing techniques for labor and delivery
- Chemical pregnancy
- Cholestasis of pregnancy
- Choline during pregnancy
- Ectopic pregnancy
- EPA & DHA for pregnancy
- Essential oils for labor and delivery
- Fertility
- Fish oil for pregnancy
- Hospital bag checklist
- How to induce labor naturally
- How many weeks is a pregnancy
- Iodine deficiency
- Iodine in pregnancy
- Normal iron levels during pregnancy
- Pregnant mom’s stress can affect baby’s microbiome
- Pregnancy spotting
- Pregnancy symptoms
- Pregnancy test
- Prenatal vitamins
- Tylenol use during pregnancy
References
(1) https://medlineplus.gov/ency/article/000909.htm
(2) https://www.hmole-chorio.org.uk/patients_info/introduction-to-molar-pregnancy/
(3) Ghassemzadeh S, Farci F, Kang M. Hydatidiform Mole. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan.
(4) https://pubmed.ncbi.nlm.nih.gov/27486130/
(5) https://pubmed.ncbi.nlm.nih.gov/12798471/
(6) https://www.sciencedirect.com/science/article/pii/S2214911223000681
(7) https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-022-05004-3
(8) https://www.asahq.org/madeforthismoment/anesthesia-101/effects-of-anesthesia/
(9) https://onlinelibrary.wiley.com/doi/full/10.1002/ccr3.4738
(10) https://www.nidirect.gov.uk/conditions/persistent-trophoblastic-disease-and-choriocarcinoma
(11) https://www.cancerresearchuk.org/about-cancer/gestational-trophoblastic-disease-gtd/molar-pregnancy/risks-causes