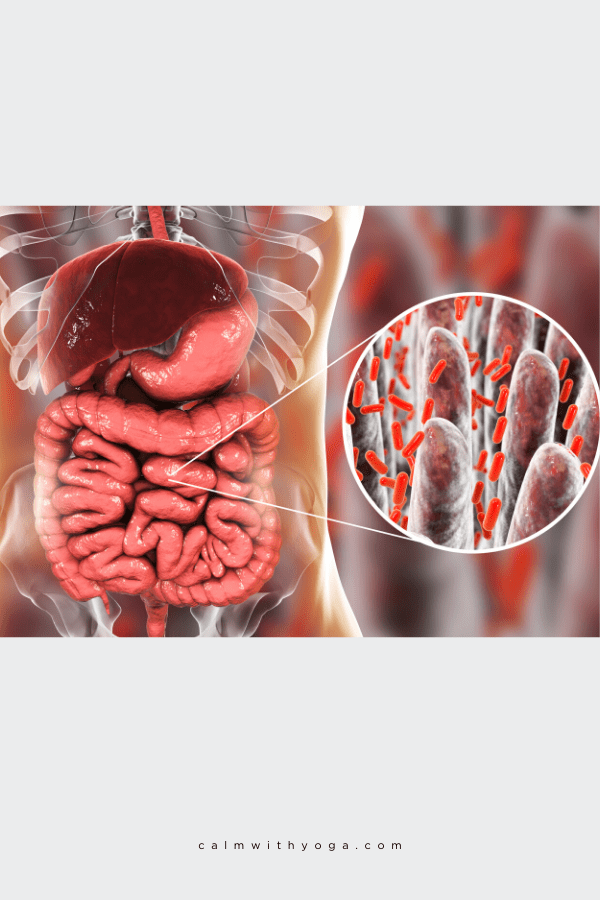
Did you know that the insides of your intestines house an entire universe of microscopic gut bacteria and other single-celled organisms?
Your gut contains approximately 100 trillion intestinal microbiota (gut flora).
This is known as the human gut microbiome.
Some of the gut bugs found in the human microbiome are beneficial to our physical and mental health.
We call these types of bacteria “commensal” gut bacteria.
This means we live in a symbiotic relationship with these organisms – we mutually benefit from each other.
Beneficial bacteria help us regulate our gene expression, metabolism, sleep-wake cycles, immune response, and can even protect us from viruses and infections.
The second class of gut microbes is what we call ‘harmful bacteria’ because high levels of these types of bugs can harm our physical and mental health.
Did you know that over 80% of your immune system is located in the gut too?
The gut’s immune cells work closely with your gut bugs to ensure your defenses are working in full capacity.
As with any environment or habitat, balance is needed in order to thrive and flourish.
The unseen microbiome universe is involved in a rhythmic flow of its own – we don’t have to consciously direct it to do what it has to do.
Under ‘normal’ functioning circumstances, we don’t have to oversee the relationships between our gut bugs and us.
That’s because when our body functions well and does what it needs to do without outside intervention we are in a state of homeostasis (bodily balance and equilibrium).
That means that the relationships between our gut bugs and us is symbiotic.
They are cooperative, mutually beneficial, and productive.
But thanks to our fast-paced, ever-changing world and growing unhealthy habits and lifestyle gut imbalance is very likely to occur…
Microbiome Dysbiosis: An Imbalanced Gut Microbiota Composition
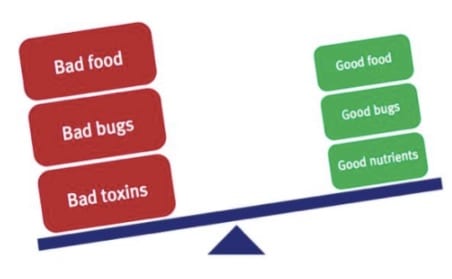
We need support from our microbes and they also need support from us in order to thrive and exist.
There is an even exchange of energy, resources, and benefits that occur in this relationship.
When the scales tip and the even exchange become uneven, dysbiosis or imbalance occurs:
“Dysbiosis is the condition of having imbalances in the microbial communities either in or on the body.
Dysbiosis is associated with many diseases, such as inflammatory bowel disease and chronic fatigue syndrome.” (1)
“Dysbiosis is a relationship of non-acute, noninfectious host microorganism interaction that adversely affects the human host.”
– Dr. Alex Vasquez, Naturopathic Physician & Functional Medicine Practitioner
Though we’re discussing microbial dysbiosis in the human gut microbiota, an imbalance can also manifest in different parts of the body.
For example:
1- Sino-respiratory dysbiosis:
Research by Mayo Clinic Proceedings found that those with acute and chronic sinusitis had higher levels of bacteria in fungus in their sinuses:
“…Of 210 patients diagnosed as having chronic rhinosinusitis (CRS), 202 patients (96%) had fungi (representing 40 different genera) in their nasal mucus.”
They also found that 100% of their control patients, including healthy individuals, also had fungi in their mucus.” (2)
2- Oro-dental dysbiosis:
There’s also a microbiome in your mouth:
It’s estimated that over 700 bacterial species reside in the oral cavity. (3)
Gum disease is the result of inflammation caused by a dysbiosis in your mouth.
3- Genitourinary dysbiosis:
Includes male and female yeast infections, UTI’s (Urinary Tract Infection), STD’s like Chlamydia, and Toxic Shock Syndrome caused by bacterial toxins.
Although microbial diversity is needed for your body’s microbiome to thrive, it needs to be the right kind.
An overgrowth of too many harmful bacteria creates dysbiosis which then creates ‘systemic inflammation’ meaning inflammation that spreads to other body parts:
“In a study of 234 patients with inflammatory rheumatoid arthritis, 44% of patients had a silent genitourinary infection.” (4)
Since inflammation is often low-grade and chronic it’s sometimes not easy to detect it unless tests are run.
Certain biomarkers like C-reactive protein can be tested for using a simple blood test.
Possible Causes of Human Microbiota Dysbiosis:
“The intestinal dysbiosis hypothesis suggests a number of factors associated with modern Western living have a detrimental impact on the microflora of the gastrointestinal tract.
Factors such as antibiotics, psychological and physical stress, and certain dietary components have been found to contribute to intestinal dysbiosis.
If these causes can be eliminated or at least attenuated, then treatments aimed at manipulating the microflora may be more successful.”
– Jason A. Hawrelak, PhD Candidate & Stephen P. Myers, PhD, ‘The Causes of Intestinal Dysbiosis: A Review’
Here are just a few possible causes:
1. Chronic anxiety, stress, & nervous system imbalance:
Are your gut problems causing your anxiety?
Or is your anxiety causing your gut problems?
Either and both can be the case.
It seems it is a ‘Catch 22’ cycle of ‘what came first.’
Multiple studies have found that exposure to psychological, physical, and social stress – even as short term as 2 hours (56) – can disrupt the balance in our guts/microbiome.
Stress creates significant reductions in elements in the mucosal lining of our intestines, which can contribute significantly to ‘pathogenic’ or ‘bad’ bacteria colonizing and overpowering the ‘good’ bacteria. (5)
An animal model psychological stress study involving maternal separation of baby monkeys found that not only does strong emotional stress disrupt the integrity of the intestinal microflora making one more susceptible to disease, but it can do so for several days thereafter. (6)
2. Crappy diet (refined sugar, processed foods, additives/preservatives):
“The quantity of refined sugar in the diet can significantly influence gut function and the composition of bowel contents,” says a study that found that diets high in simple sugars increase bacterial fermentation and bile production. (7)
“Some species of intestinal bacteria utilize bile acids as food and, hence, an increase in their production will result in a competitive advantage for this group of bacteria.” (7)
The study also found that high-carb diets slow bowel transit time.
So it takes you longer to poop your stuff out, the longer it sits inside you, the higher the risk of exposure to toxicity.
3. Antibiotic use:
It is true that antibiotics save lives in cases where they are absolutely necessary, so they definitely have their benefit and their place.
It is also true that the side effects they come with wreak havoc in our insides and present many drawbacks to our health.
They tend to be prescribed as a first go-to and even as a band-aid instead of as a last resort when all other options have been exhausted.
“Although antibiotics have significantly improved human health and life expectancy, their disruption of the existing microbiota has been linked to significant side effects such as antibiotic-associated diarrhea, pseudomembranous colitis, and increased susceptibility to subsequent disease.” (8)
My own philosophy with antibiotics is this*:
Unless it is absolutely, urgently necessary to my immediate survival and wellness, I choose to opt for other options that might prove to be as effective in solving the issue without the harsh side effects on my body.
If I should need to go on antibiotics, I’d make sure I care for my gut microbiota and help counter and minimize the effects of antibiotics to help restore balance by supplementing with high-grade probiotics such as bifidobacterium and lactobacillus.
I’d also ensure I am eating a diet rich in anti-inflammatory foods and prebiotics – undigestible fibers found in foods such as onions, leeks, apples, asparagus, and oats.
Prebiotics are considered food for beneficial gut bugs.
Both anti-inflammatory foods and prebiotics help your gut create their own short-chain fatty acids (SFCA) which help keep balance and harmony in the gut.
*This is my own personal opinion and choice. I am in no way giving advice or treatment as I am not a trained medical professional.
4. Excessive alcohol:
Excessive or regular alcohol consumption affects the amount and composition of the gut microbiota. (9)
It also imbalances our circadian rhythms.
Imbalanced circadian rhythms equal imbalanced microbiomes because the two are closely tied together.
Alcohol also disrupts the intestinal barrier function, leading to leaky gut (aka intestinal permeability). (10)
The good news is that we have the power to shift whatever imbalance may be present inside our guts.
We can alter our diets, change our relationship to food, learn to manage our stress, anxiety, and emotions more efficiently, take it easy on the weekly happy hours, and use antibiotics wisely and sparingly.
Ultimately, our mental, emotional, and physiological health is a reflection of the small and big choices we make day in and day out.
Symptoms of dysbiosis:
Here are 19 signs to look out for:
1. Anxiety/ Depression/ Moodiness
2. Brain fog/ trouble remembering and concentrating
3. Chronic bloating/gas/flatulence/belching
4. Abdominal discomfort, cramping, pains
5. Chronic heartburn/ acid reflux
6. Constipation
7. Diarrhea
8. Unexplained weight loss or weight gain
9. Micronutrient deficiencies (i.e: vitamin B6, magnesium)
10. Mucus and/or blood in stool
11. Chronic low energy/ fatigue
12. Chronic bad breath
13. The appearance of new food sensitivities
14. IBS (irritable bowel syndrome)
15. IBD (inflammatory bowel disease like Crohn’s disease or ulcerative colitis)
16. Leaky Gut (intestinal permeability)
17. Flared up or overactive immune system/ chronic inflammation/ autoimmune disease
18. SIBO (small intestinal bacterial overgrowth) – Normally there’s a relative abundance of microbes in your large intestine but when SIBO occurs there’s an overabundance of bacteria in your small intestine.
19. Chronic and unexplained nausea
REFERENCES
:
(1) http://www.nature.com/subjects/dysbiosis
(2) http://www.mayoclinicproceedings.org/article/S0025-6196(11)64228-6/fulltext
(3) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3800425/
(4) http://www.academia.edu/3862817/Nutritional_and_Botanical_Treatments_Against_Silent_Infections_and_Gastrointestinal_Dysbiosis_Commonly_Overlooked_Causes_of_Neuromusculoskeletal_Inflammation_and_Chronic_Health_Problems._Nutr_Perspectives_2006
(5) http://www.altmedrev.com/publications/9/2/180.pdf
(6) http://onlinelibrary.wiley.com/doi/10.1002/(SICI)1098-2302(199909)35:2%3C146::AID-DEV7%3E3.0.CO;2-G/abstract
(7) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1379072/
(8) http://www.annualreviews.org/doi/abs/10.1146/annurev-micro-091313-103456
(9) http://www.medscape.com/viewarticle/844190
(10) http://www.alcoholjournal.org/article/S0741-8329(14)20121-2/abstract